This is a long story and I am starting at the other end, but Its the the most current and if I feel up to it, I’ll fill in the significant events leading up to this week later.
This is a long story and I am starting at the other end, but Its the the most current and if I feel up to it, I’ll fill in the significant events leading up to this week later.
I arrived at the Hallwang Oncology clinic four days early, having cancelled TACE #5 with prof. Vogl. The reason for the cancelation was the preliminary acceptance into an ALPPS trial in the Czech Republic. (That in itself is one hell of a story, but more on that later.)
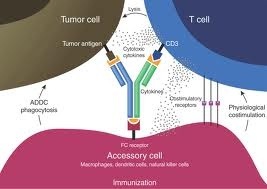
The plan for this Hallwang stay was simple. No liver directed therapies like Mytomicin or Removab, just a gentle week of liver and immune therapies to prepare my body for the complex liver surgery. What could go wrong right? (And the answer to that question, considering that it is me we are talking about, is pretty much Everything).
I arrived at Hallwang still very bloated, with high bilirubin levels manifesting in the yellowing of my eyes. I still had not recovered from the last Removab treatment and bilirubin had not been draining into the digestive system as it should. This causes pale yellow almost white stool and dark orange urine as the kidneys struggle to clear it from the system. I had hoped to get this fixed with liver support IVs at Hallwang.
The first day’s blood test showed high CRP (measure of inflammation) and because my liver had been swollen and sore as well, the Hallwang doctors deducted that I still had a liver infection and prescribed a three day course of antibiotics. I was not happy about that as the chronic bloating I now have I developed after the last round of antibiotics and it only just started to get better. As I expected the bloating got much worse again soon after the new antibiotic course was started and I was miserable.
I was given various drugs and preparations to treat the bloating symptoms, (with little help or relief), but what I really wanted was to find and fix the cause. I knew it had to be either a bacterial, yeast or fungal infection of some sorts. So I pushed for more tests. The results eventually came back and helicobacter pylori was found in the stool and blood. The treatment prescribed was a 7 day course of antibiotics. The doctors however ignored the Clostridium Defficile infection that had been found a few weeks earlier and giving antibiotics to treat the helicobacter could have been a recipe for disaster had it still been in my system, which I thought likely. I brought this to the Doctor’s attention, they did some more research and the antibiotics were changed to also account for Clostridium. You really need to be on the ball and question everything.
During my last stay at Hallwang, I had the silly idea of having my blood tested for heavy metals. This decision would now come back to haunt me. What they wound was a high level of Aluminium in my system. Almost ten times the normal upper range. I had no idea where this came from, but was told that with Australian patients they see this quite often and they believe it is in the local water. I personally think Australians in general use more antiperspirants than the europeans as is quite evident in any public place on a hot summer’s day. But whatever the source, a round of EDTA chelation therapy was recommended and I had it the next day.
The chelation therapy consisted of two large (and I mean large) volume infusions of EDTA and various minerals to replace those that the chelation will leach out along with the heavy metals. The first sign that something was wrong came during the night. With the volume of infused liquids, I expected to spend half the night passing urine, as I usually do after heavy infusion days. This time there was nothing. I woke up feeling much more bloated than before, but I did not connect the dots at that time.
The day after the bloating got much worse and my thighs swelled up as well to maybe 3 times the usual size. I weighed myself in the morning and discovered that I was 8 kilograms heavier than I should have been. I connected the dots then and had an ultrasound done. It pretty much confirmed what I suspected already. Ascites with at least 7 litres of liquid in my peritoneum. Combine that with the bloating and the swollen liver, I was one miserable pregnant whale. I can’t say whether this resulted from the chelation, or whether it is just my liver failing, but I don’t believe in coincidences. The treatment prescribed were diuretics to try and expel the liquid. That did not work, and the next morning I woke up (morning for me has become 3am), things were worse and I gained another kilogram of weight.
At this point I could not bare things any longer and a puncture was planned to drain the liquid. It seemed simple, stick a needle in, drain 6-7 litres of fluid and you end up with instant relief. The danger however is piercing the colon in the process. That would be bad, very very bad. With my luck, you can probably imagine already what happened.
Well it didn’t happen, but I got no relief either. The bacterial bloating I had also been suffering from had distended my colon. It was very close to the walls and there was very little space to insert the needle to access the fluid safely. The doctor had a go and punctured my abdomen, but got concerned (or scared) and aborted the procedure after the initial puncture yielded no fluid and she did not dare to go deeper. That was maybe a good thing, but I really needed a solution especially since my liver surgery is due in a week and the ascites put the surgery in doubt. I was given a horse dose of diuretics, but again these had little effect on the ascites and I continued to be in pain and miserable. I don’t like pain killers, but I had to take them daily now in order to get just a few hours sleep.
The following day things did not improve and I had to leave Hallwang as was due in the Czech Republic for surgery prep. I was given an elephant’s dose of diuretics and a urine bottle for what I expected to be a 4 hour drive to Plzen. This turned into a 7 hour nightmare which I will not go into. So this is where I am now, at a hotel in Plzen, the half way point on my road trip to Ostrava. It is 3am and the bloating and pain make it hard to sleep. I have a five hour drive still ahead of me, and am really hoping that the traffic will be better. The good news is that the diuretics did help a little bit, so I will continue to take oral diuretic tabs and hope that the ascites clear up on their own. I have 5 days left to get these under control.
Other treatments while at Hallwang included a stem cell injection to help my liver, hormones to try and reverse my cachexia and my least favourite, dexamethasone to help with the liver swelling.
To summarise, this time I am leaving Hallwang with a 7 day course of 3 different antibiotics to treat my gastro issues. I am taking strong diuretics daily. I am still bloated from gas, I have at least 5-6 litres of fluid due to ascites, my liver is swollen and painful. Also suffering from cachexia, having lost most of my muscle mass now. My bilirubin levels took another dive, reaching 3.2, the highest level I ever had. What’s next?
 Three weeks into my latest ketogenic diet, things took a turn for the worse. For about 8 days I suffered from what felt like severe hypoglycaemia. I had no energy what so ever and even getting out of bed to walk to the toilet became a major struggle. At the same time, my liver function tests took a dramatic turn for the worse, with many values four times higher than my worst past results.
Three weeks into my latest ketogenic diet, things took a turn for the worse. For about 8 days I suffered from what felt like severe hypoglycaemia. I had no energy what so ever and even getting out of bed to walk to the toilet became a major struggle. At the same time, my liver function tests took a dramatic turn for the worse, with many values four times higher than my worst past results.